History of Medicine, Neurology and Psychiatry
NEUROLOGY AND PSYCHIATRY IN BABYLON
I first met James Kinnier Wilson, Professor of Assyriology at Cambridge University, at King’s in 1987 at a scientific and social commemoration of his father, Samuel Alexander Kinnier Wilson (1878-1937), the distinguished National and King’s neurologist who described Wilson’s Disease, on the 50th anniversary of his death. James drew my attention to a Babylonian ‘textbook’ description of epilepsy in the British Museum.
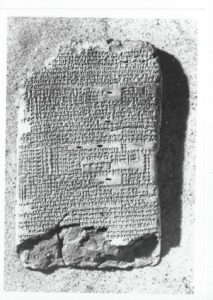
Over the next 30 years we collaborated in translating Babylonian descriptions of epilepsy, stroke, facial palsy, psychoses, obsessive compulsive disorder (OCD), phobias, psychopathic behaviour, depression and anxiety in texts from museums in London, Paris, Berlin and Istanbul. Most of these accounts date from the first Babylonian dynasty of the first half of the 2nd millennium BC, within a millennium and a half of the origin of writing. The Babylonians were remarkably astute and objective observers of medical disorders and human behaviour, but they had no knowledge of brain or psychological function. Some disorders such as stroke had a physical basis requiring the attention of a physician or asû; others, such as epilepsy or depression were viewed as supernatural due to evil demons or the anger of personal gods, requiring the intervention of the priest or ašipu; some such as OCD or psychopathic behaviour were regarded as a mystery. These remarkably detailed descriptions which are surprisingly similar to modern 19th and 20th century AD textbook accounts extend the history of these disorders by about a millennium from Greece to Babylon. The Babylonians were the first to describe the clinical foundations of what we call neurology and psychiatry.
Key References:
Kinnier Wilson J.V., Reynolds E.H.: Translation and analysis of a cuneiform text forming part of a Babylonian treatise on epilepsy. Medical History 1990; 34: 185-198.
Reynolds E.H., Kinnier Wilson J.V. Neurology and psychiatry in Babylon. Brain 2014; 137: 2611-2619
Kinnier Wilson’s 1924 Film of Patients with Movement Disorders

Through my collaboration with James KW, son of SAKW (see above), a remarkable film of patients with movement disorders has come to light. The 20 minute silent film with captions by SAKW includes patients with senile tremor, Parkinson’s disease and post-encephalitic parkinsonism, hemiballismus, Huntington’s chorea, Sydenham’s chorea, hysterical palsy and tremor, multiple sclerosis and progressive lenticular degeneration (Wilson’s disease), the latter including a brief shot of SAKW himself. The patients are filmed in Queen Square, outside the National Hospital. This is the oldest surviving film of neurological patients in the UK apart from a 1918 military film of patients with hysteria (‘war neuroses’ or ‘shell shock’) in the British Film Institute. SAKW may have been stimulated and facilitated to make this film through his friendship with Charlie Chaplin.
THE HISTORY OF EPILEPSY: MILESTONES IN 4,000 YEARS
As a specialist in epilepsy I have become increasingly interested in the history of the disorder which can be traced over 4,000 years from the earliest Babylonian descriptions (see above). In ancient civilisations, including Babylon, Greece and Rome, the mysterious, intermittent and dramatic manifestations of epilepsy were viewed as supernatural in origin. Hence the Greek work ‘seizure’, implying control by gods or evil spirits. Although the Greek Hippocrates first suggested that epilepsy was not a ‘sacred disease’, but had a natural origin in the brain, supernatural views continued to dominate until the concept of epilepsy as a brain disorder took root in Europe in the 17th and 18th centuries. In the 19th century epilepsy was gradually separated from other paroxysmal movement disorders and vascular theories were replaced by electrical ‘discharge’ theories, beginning with Robert Bentley Todd and confirmed later by Hans Berger, as described below.
In the 20th century the classification of epilepsy into different age-related syndromes and the separation of idiopathic from symptomatic or focal epilepsy, based on cortical localisation and brain networks, have continued to be debated. New investigative techniques, such as video-telemetry or CT and MRI imaging have greatly improved diagnostic precision. An increasing number of antiepileptic drugs and the use of neurosurgical techniques for selected cases has improved outcomes, but basic mechanisms are still far from understood and approximately one-third of patients with epilepsy continue to experience recurrent seizures.
With such a prolonged history of ignorance, misunderstanding, isolation and stigmatisation the psychosocial consequences and comorbidities of epilepsy have received increasing attention. Epilepsy is a global medical, public health and social problem. The International League Against Epilepsy(ILAE) was founded in 1909 and the International Bureau for Epilepsy(IBE) in 1966. The ILAE/IBE/WHO Global Campaign Against Epilepsy to improve diagnosis, treatment and care, especially in developing countries, was launched in 1997. The Campaign continues to gather momentum as described above and is the latest milestone in the history of epilepsy.
Key References:
Reynolds E.H., Trimble M.R. The Bridge between Neurology and Psychiatry. Churchill Livingstone, 1989.
Reynolds E.H. Milestones in epilepsy. Epilepsia 2009; 50: 338-342.
Reynolds E.H. Epilepsy and Neuroscience : Evolution and Interaction Frontiers in Neuroanatomy 2020, doi: 10.3389/fnana.2020.00025
HYSTERIA ANCIENT AND MODERN: BRAIN AND MIND
The word ‘hysteria’ originated in the Corpus Hippocraticum (c 420 BCE) as a natural explanation for a variety of diseases in women linked in theory to an animate or inanimate womb, but which in the last five centuries has evolved to describe an elusive disorder of brain ± mind in men and women, currently often referred to as ‘functional neurological disorder’. Babylonians, Assyrians and Egyptians had no knowledge of brain or psychological function. Babylonian and Assyrian descriptions of disease and behaviour include only rare examples suggestive of modern hysteria. The Greek and Roman civilisations had some knowledge of neuroanatomy, but little of nervous system function, conceived in terms of humours. Examples of modern hysteria are infrequent and fragmentary, the most plausible being attempts to separate epilepsy (the sacred disease) from other forms of loss of consciousness.
The study of hysteria in ancient civilisations adds interesting insight into the evolution of thinking about brain, psyche, mind and self. Babylonian and Egyptian medical and behavioural descriptions are objective, based on detailed observation. Greek and Roman accounts include some subjective aspects, probably linked to early attempts to understand identity, the psyche, intellectual and emotional functions. The great debate about whether the latter resided in the head/brain (Plato) or the heart (Aristotle) has only been settled in the last few centuries, during which hysteria also became linked to brain ± mind. More recent increasing knowledge of brain function has been accompanied by increasing interest in subjective feelings, thoughts, the inner life and subconscious mechanisms, suggesting we may have become more self-aware than in earlier civilisations. This in turn is reflected in evolving clinical presentations of hysteria, which are influenced by ideas and feelings and by social and cultural factors. The study of hysteria is one of the keys to a greater understanding of the relationship between brain and mind, the outstanding challenge of neuropsychiatry and of medicine.
Key References:
Trimble M., Reynolds E.H. A Brief History of Hysteria: From the Ancient to the Modern. In: Handbook of Clinical Neurology, vol 139 (3rd series). Functional Neurological Disorders (Eds: Hallett M, Stone J, Carson A). Elsevier, Amsterdam, 2016: pp 3-10.
Reynolds E.H. Hysteria in ancient civilisations: A neurological review. Possible significance for the modern disorder. J. Neurol Sci 2018; 388: 208-313.
NINETEENTH-CENTURY NEUROLOGY AND PSYCHIATRY
As described in the Section on Neuropsychiatry neurology emerged as an independent discipline from ‘nervous disorders’ or ‘neuroses’ in the middle of the 19th Century, separate from psychiatry.
Robert Bentley Todd, Michael Faraday and the Electrical Basis of Brain Function and Epilepsy
I have made a special study of Robert Bentley Todd (1809-1860), whose statue stands outside King’s College Hospital which he founded in 1840.

The statue was commissioned in 1860 in recognition of his achievements in clinical medicine, anatomy, pathology, physiology and medical education. Much less understood then or since were his contributions to neurology and neuroscience, which at that time did not exist. Todd was the first to identify the functions of the posterior columns of the spinal cord and to describe locomotor ataxia or tabes dorsalis. His ‘Clinical Lectures on Paralysis’ (1856) are a milestone in the history of stroke. His greatest achievement was in laying the foundations of our modern understanding of the electrical basis of brain function and of epilepsy in particular.
In this he was influenced by his contact with Michael Faraday (1791-1867) at the nearby Royal Institution in London, where Faraday was developing his famous concepts of the interchangeable polar forces of electricity and magnetism.
Todd was a pioneering microscopist, the first in the UK to apply Schwann’s 1839 cell theory to the nervous system. He brilliantly foresaw that each nerve ‘vesicle’ (cell) and its associated fibres (axons) were a distinct apparatus for the development of ‘nervous polarity’ or nerve cell conduction. He therefore laid the foundations of what became known decades later as the ‘neurone doctrine’.
In his 1849 Lumleian lectures he applied these concepts to a radically new electrical theory of epilepsy in which he confirmed that a rise in electrical tension in the grey matter of the brain could lead to a sudden discharge, similar to the phenomenon ‘described by Faraday under the name of ‘disruptive discharge’. The concept of electrical discharges in epilepsy were not widely accepted until nearly a century later with the discovery of the human electroencephalograph by Hans Berger (1873-1941) in the 1920’s by which time Todd’s discoveries and accounts had been forgotten or overlooked. Todd was the UK’s greatest neurologist prior to the establishment of neurology in this country with the foundation of the National Hospital for the Paralysed and Epileptic in 1860, the year of his death.
Key References:
Reynolds E.H. Todd, Faraday and the electrical basis of brain activity. Lancet Neurol 2004; 3:557-563.
Reynolds E.H. Jackson, Todd, and the concept of ‘discharge’ in epilepsy. Epilepsia 2007
Anglo-French Neurological Interactions in the Nineteenth and early Twentieth Centuries
The development of neurology as an independent discipline in the mid 19th century was considerably influenced by the almost simultaneous foundation of the National Hospital for the Paralysed and Epileptic in London and the Salpêtriere School initiated by Jean-Martin Charcot (1825-1893) in Paris in the 1860’s. With my French neurological colleague, Emmanuel Broussolle, we have recently studied seminal interactions prior to and following the establishment of these Schools up until World War 1. Earlier interactions involved Graves, Todd, Laycock and Allbutt in Britain and Trousseau and Duchenne in France. The French C.E. Brown-Séquard was one of the first two physicians appointed to the National Hospital. Charcot made numerous visits to Britain and presentations to British Medical Association meetings, while many National Hospital and other physicians visited the Salpêtriere. Benjamin Ball, an Englishman, was the first Professor of mental and brain diseases in Paris. Hughlings Jackson profoundly influenced French views on epilepsy and cortical localisation. Alexander Bruce in Edinburgh and S. A. Kinnier Wilson in London maintained frequent contacts with Paris, where the latter first presented his famous thesis on hepatolenticular degeneration, later known as Wilson’s Disease. Many interactions were created by the International Medical Congresses in London and Paris of 1881, 1900 and 1913 and by the Entente Cordiale of 1904.
The London Neurological Society, founded in 1886, had many interactions with the Société de Neurologie de Paris, founded in 1899. Likewise many French authors contributed to the journal, Brain, founded in 1878, but relatively fewer British physicians published in Revue Neurologique (1893) or its precursors, although 14 were elected corresponding members of the Société de Neurologie de Paris by 1914.
Our review illustrates the constructive influence of the British and French Schools on each other and thus on the development of neurology. The clinico-pathological studies of the Salpêtriere were complemented by the clinical assessment skills of the physicians of the National Hospital. Although neuropathology developed later in London, the establishment of neurosurgery there by Victor Horsley influenced its subsequent development in Paris.
Key References:
Reynolds E.H., Broussolle E. Allbutt of Leeds and Duchenne de Boulogne: Newly discovered insights on Duchenne by a British neuropsychiatrist. Rev. Neurol.(Paris) 2018; 174:308-312
Broussolle E., Reynolds E.H. Anglo-French neurological interactions in the 19th and early 20th centuries: Physicians, Places and Events. Rev. Neurol (Paris) 2021; 177: 859-870
Reynolds E.H., Broussolle E. Anglo-French neurological interactions in the 19th and early 20th centuries: Societies and Journals. Rev. Neurol (Paris) 2022; 178; 291-297
Yorkshire’s influence on the Understanding and Treatment of Mental and Neurological Diseases in the Nineteenth Century
With my psychiatric colleague, Henry Rollin, we have studied the considerable influence of Yorkshire physicians and reformers on the care of the insane in 19th century Britain. At the turn of the century a more humane approach to the mentally ill, disabled and destitute was stimulated by the Reform Movement, initially at The Retreat in York, founded and developed by the Quaker Tuke family.
These early aspirations were later overwhelmed by industrialisation, urbanisation and the scale of the need, such that most new asylums soon became gigantic institutions for chronic insanity. In addition to The Retreat two other institutions in Yorkshire remained beacons of enlightenment in the general gloom of Victorian alienism. One was the West Riding Lunatic Asylum in Wakefield, led by Sir James Crichton-Browne (1840-1937), who initiated seminal neurophysiological and neuropathological research into brain and mental diseases. The other was the Leeds Medical School and Wakefield axis associated with Sir Thomas Clifford Allbutt (1836-1925), which pioneered the teaching of mental diseases and later the first Chair of Psychiatry. Three other Yorkshiremen who greatly influenced 19th century neurology and psychiatry were Thomas Laycock (1812-1876) in York and Edinburgh and both John Hughlings Jackson(1835-1911) and Henry Maudsley in London. See section below.
Key Reference:
Rollin H.R., Reynolds E.H. Yorkshire’s influence on the understanding and treatment of mental diseases in Victorian Britain: The golden triad of York, Wakefield and Leeds. J.Hist. Neurosci. 2018; 27:72-84
John Hughlings Jackson and Thomas Laycock
The place of John Hughlings Jackson (1835-1911) in the history of neurology is well established, based on his extensive writings on many neurological subjects, especially epilepsy, paralysis, movement and speech disorders, cortical localisation, brain and mind.

Much less well known is Thomas Laycock (1812-1876) who first interested Jackson in the nervous system as his teacher at the York Medical School and who wrote extensively about nervous disorders, brain and mind himself.
As Jackson moved south to London in 1855/1856 Laycock moved in the opposite direction to become the first Englishman appointed to the most prestigious Chair of Medicine in the UK at Edinburgh. Jackson was profoundly influenced by Laycock’s 1845 theory of the reflex functions of the brain, so much so that he continued to view the brain as an exclusively sensorimotor machine. Although he saw the brain as the organ of mind he viewed mental states as intrinsically different, occurring in parallel with correlative nervous states, but without any causal interaction between them, ie his ‘doctrine of concomittance’. Laycock however did not consider that all human behaviour was reflex and he saw his theory as opening the door to ‘unconscious cerebration’. Furthermore, unlike Jackson, he separated ‘mind’ from ‘consciousness’ and saw mind as causally linked to brain through physics, biology and vital forces (energy). He viewed mental diseases as brain diseases and urged the study of mind in health and insanity by medical science. For this he established in Edinburgh the first ever University course on ‘Medical Psychology and Mental Diseases’ and taught a distinguished generation of neurologists and psychiatrists, including three of the later founding editors of the journal Brain.
Although Jackson and Laycock both took an evolutionary view of brain and mind, Jackson never referred to Laycock’s earlier scientific concepts, relying instead on the evolutionary concepts of the philosopher Herbert Spencer (1820-1903). Laycock’s views on brain and mind are nearer to modern neuroscientific concepts than those of Jackson. If some view Jackson as the father of British neurology, Laycock has some claim to be considered the father of British neuropsychiatry.
Key Reference:
Reynolds E.H., John Hughlings Jackson and Thomas Laycock: Brain and Mind. World Neurology, Aug/Sept 2023, pages 4-5.
Reynolds E.H., John Hughlings Jackson and Thomas Laycock: Brain and mind. Brain 2020;143:711-714
HOW TO AVOID HARMFUL NATIONAL QUARANTINES: A HISTORICAL PERSPECTIVE
Why has the UK recently experienced three very harmful national quarantines for a pandemic for the first time in over 150 years? Such quarantines were formally abandoned in 1877 as impractical without serious economic and social consequences, as indeed we have witnessed. Following the 1875 Public Health Act quarantines were replaced by a system of primary care-led local public health, which protected this country throughout the 20th century from numerous epidemics and pandemics, as illustrated during and after World War 2 in the village of Caerleon, where my father, a single-handed General Practitioner, was also the local Medical Office of Health working closely with the local Council.
Regrettably in the 21st century local public health was progressively eroded and centralised, such that when the covid 19 pandemic struck local public health defences for an infectious disease no longer existed. This combined with the fragility of the NHS left the country particularly vulnerable and the first national quarantine was unavoidable. Unfortunately the Government failed to learn the lessons of history or of more successful countries. Instead it made the monumental misjudgement of establishing an inadequate new centralised test, trace and isolate system, run by private companies with little or no experience of public health, and it failed to rebuild local public health defences, thus resulting in two further harmful national quarantines. History and present experience indicate that to prevent further such disastrous quarantines in the future the way forward is to revive a modernised partnership between primary care and more granular local authority structures with the guidance and support of central government.
Key References:
Reynolds E.H. Primary Care and the prevention of harmful national quarantines. BJGP Life, May 21st 2021
Reynolds E.H. How to avoid harmful national quarantines: primary care led local public health: a historical perspective. JRSM 2022; 115: 12-15
NATIONAL HEALTH SERVICE OR NATIONAL HEALTH BUSINESS: AN HISTORICAL PERSPECTIVE
In 54 years on the frontline at tertiary, secondary and primary levels I have experienced the best and the worst of the NHS. It is clear to me that standards of service and care have been falling since the 1990 NHS and Community Care Act, which introduced a profound change in NHS structure and culture, when best Service practice was subordinated to or in tension with best Business practice. This led to fragmentation and loss of coordination, communication and continuity of care; the expansion of an enormous and increasingly centralised bureaucracy with constant strain between frontline staff and management at all levels; together with much greater financial inefficiency. In a nutshell the NHS became the NHB. Since then the NHS has rarely been out of the news with concerns about underfunding, understaffing, patient safety and staff morale. The capacity of the NHS has been steadily falling in relation to the increasing demands upon it, now greatly aggravated by the pandemic.
Solutions include: (1) abolition of the internal market; (2) a return to professionally-led locally organised and integrated physical, mental and social/community services, related to local needs; (3) the reintroduction of collaboration and continuity of care; (4) local professional providers of services, supported by their professional Colleges and Associations, should accept responsibility for driving and maintaining the highest clinical standards in place of the present more remote, conflicted political/managerial and financial interests. Only then will we know whether the country can afford or is willing to pay for a Service of the highest standard, or whether the service should be rationed. In a better future for the NHS both clinical and financial efficiency will be more readily aligned with or without some overt rationing, in place of the present combination of lower clinical standards and financial inefficiency.
Key References:
Reynolds E.H. A better future for the NHS: An historical perspective from the frontline. JRSM 2018; 111:374-376
Reynolds E.H. National Health Service or National Health Business? An historical perspective. Royal College of Physicians: Commentary 2019; 4: 20-22.
NHS Health Warning
Extract from the Times on Friday 23rd December 2022
Sir,
I worked for 54 years in the frontline of the NHS at tertiary, secondary and primary levels (Health Warning, December 21st). It is clear to me that standards of care have been falling since the NHS and Community Care Act of 1990, when Service principles were subordinated to or in constant tension with Business and market principles. Since then the NHS has become increasingly centralised and bureaucratic. Collaboration, communication and continuity of care have been undermined, with increasing concerns about patient safety and staff morale, aggravated by increased demands and inappropriately reduced capacity. Among the solutions should be a return to a predominantly professionally led and locally organised Service with Government support as envisaged and implemented by Aneurin Bevan and the founders of the NHS.
Edward Reynolds
Dr. Edward H. Reynolds MD FRCP FRCPsych
Former Consultant Neurologist to the Maudsley and Kings College Hospitals, Epsom Hospital and the Integrated Care Partnership, Epsom.
HEALTH EFFECTS OF POOR HOUSING
Medical profession has a role
Extract from British Medical Journal on 20th May 2023
Dear BMJ Editor,
Dobson asks why it’s fallen to the medical community to act on the detrimental health effects of poor housing (Editor’s Choice, 1 April).
For most of the past century the medical profession has acted on the effects of poor housing. My father, a GP, was the medical officer of health for an urban district council in Monmouthshire. He worked with two councillors to ensure the health of the community in the home, school, and workplace. Annual reports from medical officers of health improved local housing and influenced housing policy.
Sadly, public health has been greatly run down and centralised. Medical officers of health no longer exist, and GPs rarely visit homes. Taking a social history was one of the first things I learnt in medical school. There is, and should be, a role for the medical profession in acting on the health effects of poor housing. The profession needs reminding of this.
Edward H. Reynolds, consultant neurologist, London